
Introduction: Why Legal Knowledge Empowers Healthcare Assistants
Imagine this: a healthcare assistant (HCA) unintentionally breaches patient confidentiality by discussing a resident’s condition in a public area. The result? A formal complaint, disciplinary action, and a shaken sense of professional confidence. This is just one example of how misunderstanding the duty of care can lead to serious consequences—not only for patients, but for the HCA’s career and reputation.
This guide breaks down the concept of duty of care, outlines the legal responsibilities specific to UK healthcare assistants, and offers practical advice to stay compliant, confident, and protected in your role.
What Is Duty of Care in UK Healthcare?
Duty of care is the foundation of safe, ethical, and compassionate healthcare. For UK healthcare assistants (HCAs), it means acting in the best interest of patients at all times, ensuring their safety, dignity, and wellbeing.
In legal terms, the duty of care refers to the obligation to avoid actions that could reasonably be foreseen to cause harm. This applies to every interaction with patients, whether you’re assisting with mobility, supporting personal hygiene, or simply offering a listening ear.
Even though HCAs are not regulated by the Nursing and Midwifery Council (NMC), they are still accountable under UK law and employer policies. That means if a patient is harmed due to negligence, poor communication, or failure to follow procedures, the HCA may be held responsible.
Why It Matters:
- It protects patients from harm, neglect, and abuse.
- It protects you from legal trouble or disciplinary action.
- It builds trust between you, your patients, and your team.
Healthcare Assistant Training
Legal Responsibilities of Healthcare Assistants: What the Law Expects
As a UK Health Care Assistant (HCA), you may not be regulated by a professional body like nurses are—but that doesn’t mean you’re exempt from legal responsibility. In fact, your actions are governed by laws, workplace policies, and ethical standards that protect both patients and staff.
Legal responsibility means being accountable for your actions and decisions while delivering care. If something goes wrong, and you didn’t follow proper procedures, you could face disciplinary action—or even legal consequences.
Key Areas of Responsibility for Healthcare Assistants
As a UK healthcare assistant, your daily tasks go far beyond physical care. Every action you take is tied to your duty of care and carries legal weight. Understanding your core responsibilities helps you deliver safe, respectful, and lawful care—while protecting yourself from mistakes that could lead to disciplinary action. Let’s break down the key areas where your responsibilities matter most:
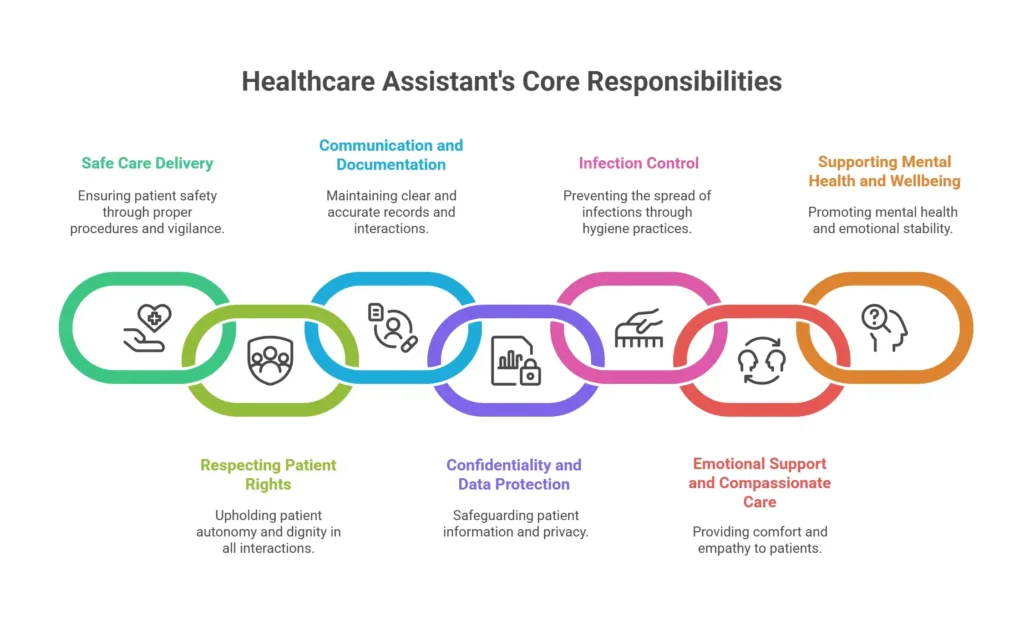
1. Safe Care Delivery
You must follow proper procedures when helping patients move, eat, bathe, or take medication (if trained). Poor manual handling or ignoring infection control can lead to injury—and legal consequences.
2. Respecting Patient Rights
Every patient has the right to dignity, privacy, and choice. You must listen to their preferences and avoid any form of discrimination or disrespect.
3. Communication and Documentation
Clear communication with patients and your team is essential. You must also document care accurately and report any changes or concerns.
4. Confidentiality and Data Protection
You must keep patient information private and secure. Sharing details without permission—even casually—is a breach of the law under GDPR.
5. Infection Control
You’re responsible for following hygiene protocols to prevent the spread of illness. This includes handwashing, PPE use, and cleaning procedures.
6. Emotional Support and Compassionate Care
Providing emotional reassurance is part of holistic care. You must treat patients with kindness, patience, and empathy, especially during distressing moments.
7. Supporting Mental Health and Wellbeing
You may be the first to notice signs of anxiety, depression, or confusion. You must report these observations to the appropriate clinical staff.
Common Legal Pitfalls and How to Avoid Them
Breaches of Patient Confidentiality and GDPR Compliance
One of the most common legal pitfalls is mishandling patient data. Discussing medical details in public areas or accessing records without authorisation violates GDPR and patient confidentiality laws in UK healthcare settings. HCAs must understand data protection protocols and maintain strict privacy standards.
How to avoid it: Always follow your organisation’s data protection protocols and only access patient information when authorised.
Infection Control Failures in Care Settings
Neglecting infection control procedures—such as improper use of PPE or poor hand hygiene—can lead to serious health risks and breach workplace policy. Infection control for HCAs is not optional; it’s a legal and professional requirement under NHS and CQC guidelines.
How to avoid it: Follow infection control for HCAs guidelines, attend regular training, and never skip hygiene steps—even when rushed.
Administering Medication Without Authorisation
Healthcare assistants (HCAs) must never administer medication unless formally trained and authorised. Administering drugs outside your scope of practice can result in patient harm and legal liability. Medication administration rules for HCAs are clearly defined and must be followed precisely.
How to avoid it: Only administer medication if you’ve received formal training and written authorisation from your employer.
Inaccurate or Falsified Care Documentation
Poor record-keeping, whether accidental or intentional, can compromise patient safety and lead to legal action. Care documentation standards in UK healthcare require HCAs to record observations and interventions accurately, ensuring continuity of care and legal protection.
How to avoid it: Record all care activities truthfully, promptly, and in line with your organisation’s documentation policy.
Failure to Report Safeguarding Concerns
HCAs are legally obligated to report suspected abuse, neglect, or exploitation. Failing to escalate safeguarding concerns can result in disciplinary action and breach safeguarding responsibilities under UK law. Timely reporting protects both patients and professionals.
How to avoid it: Know your safeguarding procedures and report concerns immediately to your designated safeguarding lead.
Ignoring Changes in Patient Condition
Not escalating changes in a patient’s physical or mental health to senior staff is a serious oversight. HCAs must be vigilant and proactive, especially when supporting mental health and wellbeing. Early intervention can prevent deterioration and legal repercussions.
How to avoid it: Monitor patients closely and report any physical, emotional, or behavioural changes to senior staff without delay.
Performing Tasks Outside the Scope of Practice
Undertaking clinical procedures without proper training or supervision is a major legal risk. The scope of practice for HCAs in the UK is clearly defined, and stepping beyond it—even with good intentions—can result in disciplinary action or patient harm.
How to avoid it: Stick to duties you’re trained for and ask for supervision or guidance when unsure.
Improper Use of Physical Restraint
Using physical restraint without proper training or justification violates patient rights and legal standards. HCAs must follow restraint policy guidelines in healthcare settings and seek senior support when managing challenging behaviour.
How to avoid it: Only use restraint if trained and authorised, and always follow your organisation’s behaviour management protocols.
Discrimination and Breach of Equality Standards
Treating patients unfairly based on race, gender, age, or disability breaches the Equality Act 2010. HCAs must uphold inclusive care practices and avoid discriminatory behaviour, ensuring equality in patient care across all settings.
How to avoid it: Treat every patient with respect and dignity, and challenge discriminatory behaviour when you see it.
Lack of Informed Consent Before Care
Providing care without obtaining informed consent undermines patient autonomy and legal safeguards. HCAs must ensure patients understand and agree to procedures, especially in personal care or clinical support roles. Informed consent in healthcare is a cornerstone of ethical practice.
How to avoid it: Always explain procedures clearly and confirm the patient’s understanding and agreement before proceeding.
Real-Life Scenarios: Duty of Care in Action
Understanding duty of care is one thing—seeing it in action is another. These real-life examples show how healthcare assistants (HCAs) apply legal and ethical responsibilities in everyday situations, and what can go wrong when the duty of care is ignored.

Scenario 1: Ignoring a Patient’s Fall
Amira, an HCA in a care home, noticed Mr. Thompson sitting on the floor after a minor fall. He said he was fine, so she helped him up and didn’t report it. Later, he was found to have a fractured hip, and no one had documented the incident.
What went wrong: Amira failed to report and record the fall, breaching her duty of care. She received a formal warning, and the care home faced scrutiny for poor incident handling.
Lesson: Always report and document any fall or injury, even if the patient seems okay. It protects both the patient and your professional standing.
Scenario 2: Breach of Confidentiality
Situation: James, an HCA in a busy hospital ward, was chatting with a colleague during lunch. He casually mentioned that one of the patients had been diagnosed with a sexually transmitted infection. Although he didn’t name the patient, the details made it easy to identify who he was referring to.
What went wrong: A nearby staff member overheard and reported the conversation. James was found to have breached confidentiality under GDPR and hospital policy. He received a formal warning and was required to complete additional training.
Lesson: Never discuss patient information in public or informal settings—even without names. Confidentiality is a legal duty, and even casual comments can lead to serious consequences.
Scenario 3: Failure to Report Safeguarding Concern
Situation: Priya, an HCA in a care home, noticed that a resident had unexplained bruises and seemed fearful around a particular staff member. The resident hinted that someone had hurt them, but Priya wasn’t sure what to do and decided not to report it.
What went wrong: Weeks later, a safeguarding investigation revealed ongoing abuse. Priya was questioned for failing to act on clear warning signs. Although she wasn’t the abuser, her silence was considered a breach of duty of care.
Lesson: If you suspect abuse or neglect, you must report it immediately—even if you’re unsure. Safeguarding is a legal responsibility, and failing to act can put vulnerable people at risk.
Your Rights as a Healthcare Assistant
While Healthcare Assistants HCAs carry legal responsibilities, they also have rights that protect their wellbeing, professional integrity, and ability to deliver safe care. Understanding these rights helps you stay confident, supported, and legally protected in your role.
Training & Resources to Stay Legally Safe
Staying legally safe as a healthcare assistant isn’t just about knowing the rules—it’s about keeping your skills sharp and your knowledge up to date. The right training and resources help you deliver safe, confident care while protecting yourself from legal risks.

Care Certificate – Standard 3: Duty of Care
This is the foundation for all HCAs in the UK. Standard 3 covers what duty of care means, how to apply it, and how to handle dilemmas. It’s essential for anyone starting or refreshing their knowledge.
Tip: Make sure your Care Certificate is complete and up to date—employers often ask for it during recruitment or audits.
Employer Policies and Induction Training
Every workplace has its own procedures for safeguarding, confidentiality, reporting incidents, and working within scope. Your induction training should cover these—if it doesn’t, ask for clarification.
Tip: Keep a copy of your workplace’s policies and refer to them regularly. They’re your first line of defence in legal matters.
Continuing Professional Development (CPD)
CPD courses help you stay current with best practices in manual handling, infection control, safeguarding, and communication. Many are free or low-cost online.
Recommended platforms:
- Skills for Care.
- IOMH - Institute Of Mental Health.
- NHS Learning Hub.
- FutureLearn (UK-based healthcare modules)
Safeguarding and GDPR Training
Understanding how to protect vulnerable adults and handle personal data is critical. These are legal requirements, not optional extras.
Tip: Look for refresher courses every 12–24 months, especially if your role involves handling sensitive information.
Support from Supervisors and Unions
If you’re unsure about a task or situation, ask your supervisor. If you’re facing disciplinary action or need advice, unions like UNISON or the Royal College of Nursing (RCN) offer guidance and representation.
Conclusion: Stay Informed, Stay Protected
As a UK healthcare assistant, your role is more than just practical support—it’s a legal and ethical commitment to protect those in your care. Understanding your duty of care and legal responsibilities isn’t just about avoiding mistakes; it’s about delivering confident, compassionate, and professional care every single day.
Additional Resources
- Health Care Assistant (HCA) Job: Your Questions Answered
- What does Health and Social Care Mean? What are The Impacts of 6’C Values on Health and Social Care?
- The Concept of Compassionate Care in Healthcare
- How to Become a Carer in The UK?
- Benefits of Having A Care Certificate: Guide to Get It
- Care Certificate Standards 1-16: Complete Guide for New Care Workers!
- Care Giver vs Healthcare Assistant
- What is Adult Social Care? The Essential Guide for Caregivers You Can’t Afford to Miss!
- Why are Good Communication Skills Important In Health and Social Care?
- All Courses
Personal Development (1186)
 Employability (420)
Employability (420) Management & Administration (327)
Management & Administration (327)Health & Social Care (275)
 Health and Safety (272)
Health and Safety (272)Business (210)
IT & Software (192)
 Health and Fitness (190)
Health and Fitness (190) Teaching & Education (160)
Teaching & Education (160) Mental Health & Counselling (110)
Mental Health & Counselling (110) Accounting & Finance (105)
Accounting & Finance (105) Science & Technology (100)
Science & Technology (100) Sales & Marketing (92)
Sales & Marketing (92) Art & Design (83)
Art & Design (83) Construction & Engineering (83)
Construction & Engineering (83)Language (74)
 Compliance & Law (72)
Compliance & Law (72)Career Bundle (57)
 Photography & Lifestyle (44)
Photography & Lifestyle (44) Animal Care (38)
Animal Care (38) Sports & Fitness (36)
Sports & Fitness (36) Diet & Nutrition (30)
Diet & Nutrition (30)Makeup & Beauty (26)
 Food Safety & Hygine (22)
Food Safety & Hygine (22)First Aid (20)





0 responses on "Duty of Care Explained: Legal Responsibilities for UK Healthcare Assistants"